When the decision is made to be listed for transplant the waiting begins. Again this is not an easy process as you as a patient or caregiver has no control on the timing or circumstances of a donor heart becoming available. As I was told several years ago (and completely agree) if you have issues with being in control you will not do well with this process.
When the transplant takes place it represents a turning point. Being immersed in the nuances of managing a failing heart, you learn the jargon, the terms, processes, and meds involved in managing the failing heart. Once the transplant takes place, you get to wipe the slate clean and start over. Management of a heart transplant becomes a new challenge. You learn about organ rejection, immune suppression, and the ongoing management of the newly transplanted organ.
For friends and casual observers this is hoped that this is the end of the struggle. The new heart is a second chance; a new lease on life (literally). This is only partially true. Yes, the transplant can allow the patient to do many things and assume most activities that any normal person could do. However, it is critically important to remember that a transplant is a treatment and not a cure.
One of our reminders that things aren't all business as usual is coming up on Monday. Russell will be going in for his heart catheterization.
After Russell's transplant almost 7 years ago, we did these more frequently. Twice in his first year and then once very year. Once you are 5 years post transplant you graduate to the once every two year program. In short, we have done this a few times, and it still provides some challenges. The heart cath is the gold standard to determine if any rejection is taking place, to measure the performance of the heart, and to detect any coronary artery disease (which heart transplant recipients are prone to). With these test does come a significant amount of fear about the "what ifs." What if they find something? what if they detect evidence of rejection? The list goes on and on. Keep in mind that when you have been down the road of heart failure these fears are very real and are not unfounded.
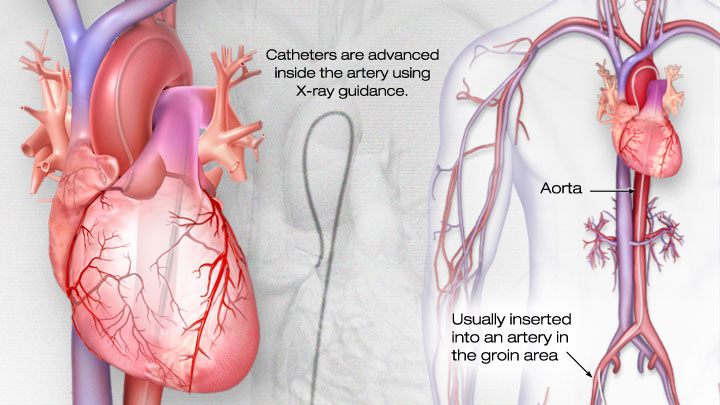
To understand a little bit more about the process. I have attached a brief description of what happens
From the American Heart Association
What is Cardiac Catheterization?
Cardiac catheterization (cardiac cath or heart cath) is a procedure to examine how well your heart is working. A thin, hollow tube called a catheter is inserted into a large blood vessel that leads to your heart. View an illustration of cardiac catheterization.
Quick facts
- Cardiac cath is performed to find out if you have disease of the heart muscle, valves or coronary (heart) arteries.
- During the procedure, the pressure and blood flow in your heart can be measured.
- Coronary angiography is done during cardiac catheterization. A contrast dye visible in X-rays is injected through the catheter. X-ray images show the dye as it flows through the heart arteries. This shows where arteries are blocked.
- The chances that problems will develop during cardiac cath are low.
NOTE: For transplant patients a biopsy is also done. They take a sample of heart tissue that will be tested for any evidence of rejection at the cellular level.
For Russell this is a day surgery procedure. Russell is now 7 and still requires full anaesthetic for the procedure. In adults, the procedure is done with a local anaesthetic so the effects are not as profound. Susan has had a heart cath in the past, and she has only vague recollections of the procedure. She was fairly "out of it."
As our cath day is coming up on Monday we have been busily preparing for the day and it is usually a very long day. There were some concerns that came up this week as Russell does have a cough. If he has any significant respiratory issues the procedure will be cancelled. Putting someone under in those circumstances is not safe and the Doctors don't take chances. We have been treating Russell with antibiotic this week in hopes that he is clear on Friday when he has is Pre Admission Clinic at the hospital. If he isn't clear the procedure will be cancelled and re-scheduled. Not a good thing for us as we have to do a great deal of preparations to make Cath Day happen. Booking time off work, ensuring Nicole has child care, and all of the appointments leading to the procedure would now have to all be re arranged if we get cancelled.
The Heart Cath is just one process we go through as part of our daily management of Russell's transplant. There are many other things we do as part of the process but the cath is one of the more significant things we do. We are hoping and praying for a good report on Friday at Russell's PAC and then an uneventful procedure on Monday.
If Susan lets me, I will be live tweeting out experience at #russellscathday I don't control what will happen that day so what I tweet will simply be our experience as it happens. I hope that informing people about our experience can help others understand how challenging managing complex health conditions can be. What we go through is similar to what many others go through as they manage their own health. It also may give some ideas about how you can support someone who has complex health issues by understanding a little of what they go through.

